How to Write Therapy Intake Notes (with Example)
Intake notes set the tone for treatment. Done well, they capture just enough history to be safe and smart, highlight the working diagnosis, and map next steps—without drowning in biography. Below is a readable structure, three real-world examples, and the exact strategies I give new clinicians on day one.
The first session is a juggle: empathy, safety, and structure—while your brain is also triaging risk and formulating care. Early in my career, I over-collected history and under-documented clinical reasoning. Audits cured that habit quickly. This guide shows you how to write therapy intake notes that are clear, defensible, and genuinely helpful for session two. We’ll connect your intake with ongoing progress notes, session-level SOAP notes, and your treatment plan.
What therapy intake notes are (and aren’t)
Intake notes document the first clinical encounter. They capture referral context, present concerns, relevant history, mental status, initial risk picture, a working diagnosis (if indicated), and an initial plan. They are not an autobiography. Your goal is to record the information that will shape care from visit two onward.
- Prioritize safety and direction: risks, protective factors, and immediate next steps.
- Decide what matters now: history that changes formulation or plan; skip the rest.
- Write for continuity: if another clinician covered your next session, they could proceed confidently.
Why intake notes matter — clinical, legal, billing
A solid intake note anchors clinical direction and demonstrates medical necessity. It protects clients (clear risks and plans), protects you (defensible documentation), and satisfies payers (active symptoms, interventions, rationale). For standards and best practices, see guidance from the American Psychological Association and SAMHSA.
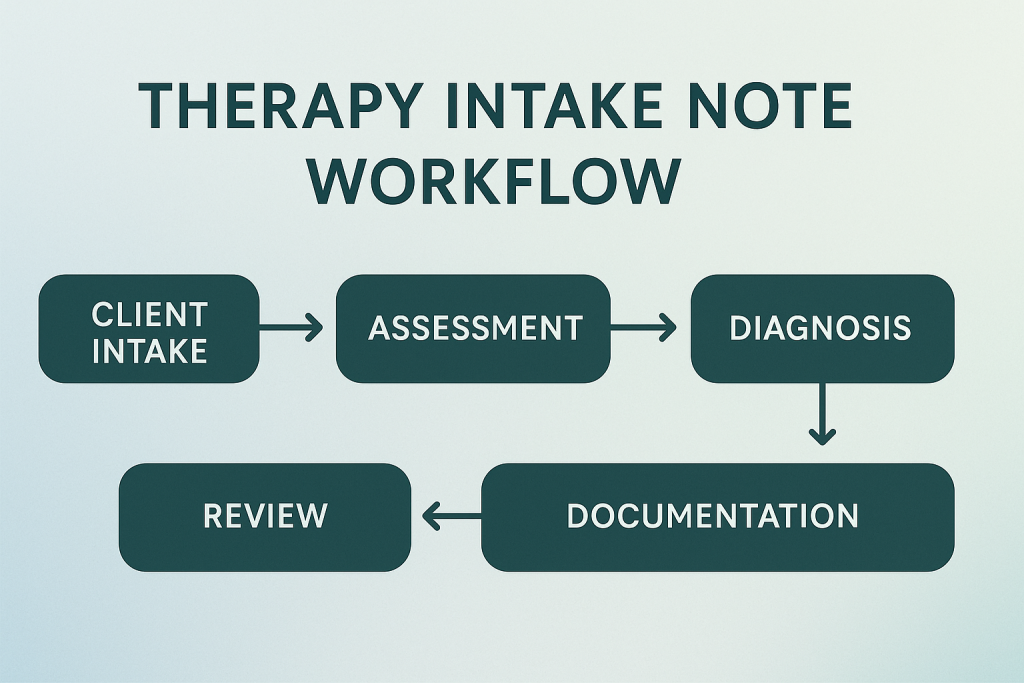
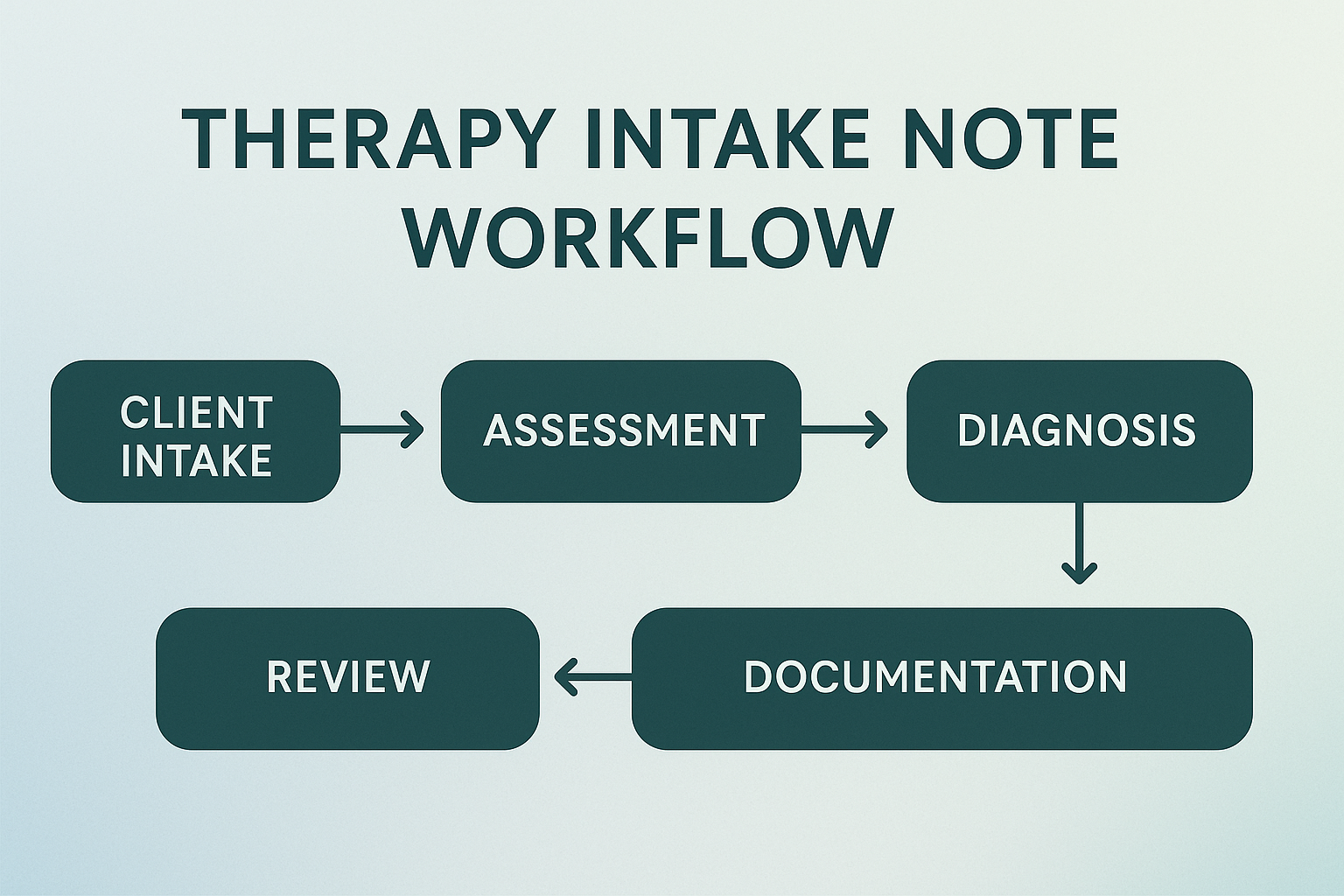
A simple, readable structure
Use SOAP if you prefer, or stick to this clear narrative outline. Either way, make each line earn its spot:
- Session details: date/time, modality (in-person/telehealth), duration, who participated.
- Referral context & presenting concerns: why now? what is most impairing?
- Relevant history: brief behavioral health history, medical, meds, family/social highlights that change care.
- Screeners & risk: PHQ-9/GAD-7 scores if used; suicidality, self-harm, harm to others, substance use; protective factors.
- Mental Status Exam (MSE): appearance, behavior, speech, mood/affect, thought process/content, orientation, insight/judgment.
- Clinical formulation: concise synthesis linking symptoms, context, and mechanisms keeping the problem going.
- Working diagnosis (if indicated): diagnostic impression + one-sentence rationale.
- Initial plan: frequency, modalities, homework, referrals, labs/med consults, safety/supervision, next steps toward a treatment plan.
From here, your ongoing documentation will live in brief, focused progress notes and session-level SOAP notes.
Therapy intake note examples (3 formats)
These examples are intentionally concise. Adjust the depth to your setting and payer requirements.
1) Individual therapy intake (anxiety)
Session: 2025-04-02, Telehealth, 60 min; client present alone. Presenting: Worry about work presentations; sleep onset delay; muscle tension; avoidance of meetings. Relevant History: Prior brief therapy in college (helpful); no psych hospitalizations; no current substances; supportive partner. Screeners/Risk: GAD-7 = 12; PHQ-9 = 7; denies SI/HI; protective factors include social support and employment stability. MSE: Neatly dressed; anxious affect; speech WNL; thought process linear; no psychosis; oriented x4; judgment/insight good. Formulation: Performance anxiety maintained by anticipatory worry + avoidance; sleep disruption exacerbates arousal. Working Dx: GAD (F41.1) — persistent worry, restlessness, sleep problems ≥6 months with functional impact. Initial Plan: Weekly CBT with exposure-based practice; 4-7-8 breathing; sleep hygiene; track triggers; next in 1 week.
2) Medication management intake (depression)
Session: 2025-04-08, Clinic, 45 min; patient present; vitals WNL. Presenting: Low mood, anhedonia, low energy x3 months; sleep fragmented; decreased appetite; no past mania. Relevant History: Family hx depression (mother); prior SSRI response (sertraline) age 24; stopped after remission; no SA; alcohol 1–2/wk. Screeners/Risk: PHQ-9 = 15 (mod); denies SI/plan/intent; protective factors: partner, work engagement; firearm access denied. MSE: Mild psychomotor slowing; constricted affect; speech soft; thought content negative self-appraisal; oriented x4. Formulation: Recurrent depressive episode without psychotic features; psychosocial stressors at work likely contributors. Working Dx: MDD, recurrent, moderate (F33.1). Initial Plan: Sertraline 25mg → 50mg in 1 week if tolerated; education on SEs; weekly therapy coordination; labs if persistent fatigue; follow-up 2–3 weeks.
3) Couples therapy intake
Session: 2025-04-15, In-person, 75 min; both partners present. Presenting: Escalating conflict cycles around chores/finances; withdrawal after arguments; diminished intimacy. Relevant History: 7 years together; 2 years married; no IPV disclosed; individual hx anxiety (Partner A). Screeners/Risk: Both deny SI/HI; no substance concerns; Gottman-style brief assessment indicates pursuer–withdrawer pattern. MSE: Both oriented x4; affect ranges from irritable to tearful; speech normal; coherent thought process. Formulation: Negative interaction cycle maintained by criticism–defensiveness–withdrawal; emotional bids missed. Working Dx: Z63.0 (Relationship distress with spouse or intimate partner). Initial Plan: Weekly couples sessions; teach softened startup + repair attempts; schedule “state of the union” check-ins; consider individual therapy for anxiety.
Time-savers & common pitfalls
- Design your intake script: a short sequence for risk, impairments, and goals keeps the interview moving.
- Write for session two: include what your future self needs to start quickly (diagnostic hunch + next step).
- Don’t overshare history: if it doesn’t change formulation or plan, leave it out.
- Document risk precisely: quotes, context, protective factors, and actions taken (safety plan, contacts).
- Connect to the plan: end with frequency, focus, and the first objective you’ll measure in the treatment plan.
- Use the same measures you’ll trend later: PHQ-9, GAD-7, or functional markers (sleep, attendance).
- Close the loop: summarize what the client is taking away and what they’ll do before session two.
Personal tip: I keep a one-page “intake cue card” at my desk—risk questions, MSE phrasing, and my three favorite opening prompts. It reduces cognitive load so I can focus on rapport.
Key takeaways
- Intake notes should prioritize safety, direction, and just-enough history.
- A concise formulation + working diagnosis points you toward a concrete plan.
- End with next steps that flow directly into your treatment plan and progress notes.
- Document risk with specifics; trend early screeners for objective change.