How to Write a Mental Health Treatment Plan
Writing a solid treatment plan is one of the most meaningful parts of therapy — it transforms insight into direction. Here’s how to do it well, efficiently, and confidently.

Writing therapy notes is one thing. But crafting a treatment plan? That’s where your clinical intuition meets structure. I still remember my first week out of grad school — sitting at my desk staring at a blank template, wondering, “How do I turn the client’s story into a plan?” Over time (and after many audits), I learned that a mental health treatment plan is less about filling boxes — and more about charting a course. In this article, we’ll explore exactly how to write a mental health treatment plan that’s compliant, collaborative, and clinically meaningful.
Download: Treatment Plan Template (PDF)
Ready template with goals, objectives, interventions & progress measures.
What is a mental health treatment plan?
A mental health treatment plan is a structured document outlining a client’s presenting issues, therapeutic goals, interventions, and progress measures. It’s both a roadmap for therapy and a communication tool for care coordination. When you learn how to write a mental health treatment plan well, you build a bridge between diagnosis and recovery — turning “what’s wrong” into “what’s next.”
Why treatment plans matter — compliance, clarity, and care
For insurance and compliance, treatment plans demonstrate medical necessity — showing that care is active, structured, and goal-oriented. For clients, they bring transparency: a shared understanding of what therapy aims to achieve. I often tell new clinicians, “Your treatment plan is like a map. It’s not about controlling the journey, but it keeps you from getting lost.”
Core elements of a treatment plan
- Client information: demographics, diagnosis, relevant history
- Presenting problems: the client’s main concerns or symptoms
- Goals: broad, meaningful outcomes (e.g., “reduce anxiety”)
- Objectives: measurable steps toward those goals
- Interventions: specific therapeutic methods or tools used
- Progress measurement: how improvement is tracked
- Review schedule: planned updates or modifications
How to write a mental health treatment plan — step-by-step
Here’s a proven framework I use and teach to new therapists. Think of it like the clinical cousin of SOAP notes — structured, flexible, and built for clarity.
1. Start with a comprehensive assessment
Gather intake data, mental status, risk assessment, and relevant history. This informs every downstream decision.
2. Define the presenting problems
Start with the client’s language, then translate into clinical terms. Precision here reduces ambiguity later.
3. Create meaningful, measurable goals
Goals should connect directly to problems and be trackable (e.g., “Reduce daily anxiety from 8/10 to 4/10 in 8 weeks”).
4. Write SMART objectives
Specific, Measurable, Achievable, Relevant, Time-bound. Keep them realistic and behaviorally written.
5. Choose interventions and modalities
Specify your methods and cadence (e.g., CBT weekly + mindfulness homework). This shows an active plan.
6. Determine how progress will be measured
Use standardized tools (PHQ-9, GAD-7), symptom logs, or functional metrics. Document baselines and targets.
7. Plan regular reviews
Re-evaluate every 30–60 days; adjust goals and interventions as needed. Document rationale for plan changes.
Example treatment plan
Client: Sarah T. | Diagnosis: GAD (F41.1)
Presenting Problem: Excessive daily worry, restlessness, sleep issues.
Goal: Reduce anxiety and improve daily functioning.
Objectives:
- Learn and use three grounding techniques within 4 weeks.
- Maintain sleep hygiene journal, reducing awake time to <30 min nightly.
Interventions:
- CBT focused on cognitive restructuring.
- Weekly mindfulness training.
- Sleep hygiene psychoeducation.
Progress Measurement:
- GAD-7 scores biweekly, journal review, and therapist observation.
Review: Every 45 days.
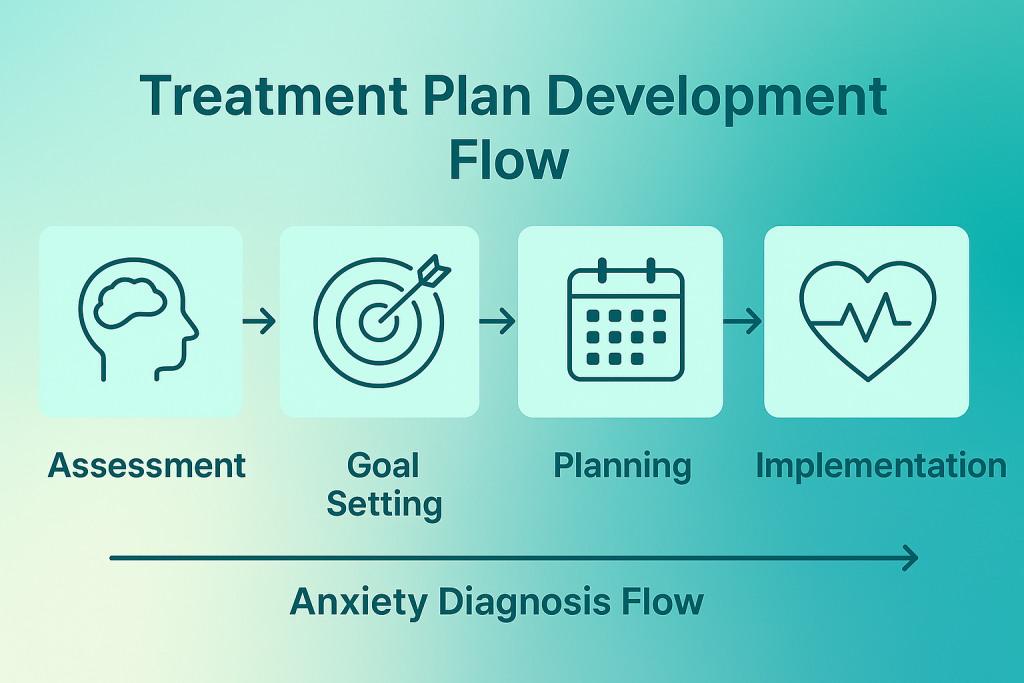
Treatment plan development flow

Tips, insights, and strategies
- Co-create with clients; shared ownership improves adherence.
- Write as if another clinician will take over tomorrow — clarity beats shorthand.
- Use the same scales insurers expect (PHQ-9, GAD-7) to show objective change.
- Document cultural and contextual factors that shape goals and engagement.
- Set calendar reminders to revisit plans monthly; avoid compliance gaps.
Key takeaways
- Clear treatment plans align care, compliance, and client trust.
- SMART objectives keep therapy focused and measurable.
- Review dates ensure timely progress checks and adjustments.
- Regular outcome tracking supports claims and continuity of care.
Need a treatment plan tailored to your practice?
Our clinical team can customize templates, goals, and workflows to match your caseload and payer mix.
Talk to a Practice ConsultantFrequently asked questions
How long should a mental health treatment plan be?
How often should plans be updated?
Can clients see their plan?
What if a client’s goals change mid-treatment?
Should I use a template?
Are plans required for all clients?
How is progress measured?
Should I include client strengths?
Is handwriting acceptable?
How to write a mental health treatment plan efficiently?
Author & Reviewer

TherapyDial Editorial Team
Clinical review by licensed therapists to ensure accuracy, clarity, and compliance.