How to Write Progress Notes — Clear, Compliant, and Fast
Progress notes should tell the story of care without eating your evening. Below is the structure I’ve refined over a decade: a reliable flow, clinician-tested examples, and practical strategies you can use today.
Writing in a personal journal has no rules. Progress notes do. They serve compliance, continuity, and client outcomes. Early in my career, I tried to make every note perfect on the first pass — and burned a lot of time. What finally worked: a two-step rhythm (a quick note right after session, then a short finalize block once a day) and a structure that balances clarity with brevity. This guide shows you exactly how to write progress notes that stay tight, defensible, and truly useful. You’ll also see how progress notes connect with your session documentation like SOAP notes and long-view planning in treatment plans.
What progress notes are (and aren’t)
A progress note is the concise record of a visit: what brought the client in today, what happened in session, how the client is doing relative to their goals, and what happens next. It differs from a treatment plan (which sets long-term goals and measurable objectives) and from a SOAP note (a specific note format). Your progress note can use SOAP or another structure — the point is to document today’s clinically relevant change and the rationale behind your next steps.
- Signal over noise: Keep every sentence tied to diagnosis, progress, risk, or plan.
- Continuity first: Write so another clinician could step in tomorrow and orient fast.
- Defensible: If you changed course, say why. If you held steady, say why.
Why progress notes matter — clinical, billing, legal
Progress notes protect clients and clinicians. Clinically, they track outcomes and inform the next session. For billing, they demonstrate medical necessity (active symptoms, interventions, and response). Legally, timely and specific notes create a defensible record — especially around risk assessment and safety planning.
As a rule, I document what changed since last time, what I did, and why that matters for care. That simple trio keeps notes short, readable, and audit-ready.
A structure that works in the real world
Whether you write in SOAP or a simple narrative, these are the essential blocks for a high-quality progress note:
- Session context: date/time, modality (in-person/telehealth), and any constraints (late arrival, tech glitches).
- Present focus: a crisp line or two about why they came today and what changed since last time.
- Interventions: what you actually did (e.g., cognitive restructuring on worry thoughts; breathing retraining; trauma processing).
- Client response: observable changes, quotes or metrics (e.g., “GAD-7 decreased from 12→9”).
- Clinical impression: your synthesis — improving, stable, or worsening; diagnostic reasoning if relevant.
- Plan: next session cadence, homework, referrals, risk/safety updates, treatment-plan alignment.
If you prefer an explicit SOAP envelope, map the same content to Subjective → Objective → Assessment → Plan. We cover SOAP structure in detail here: How to Write SOAP Notes.
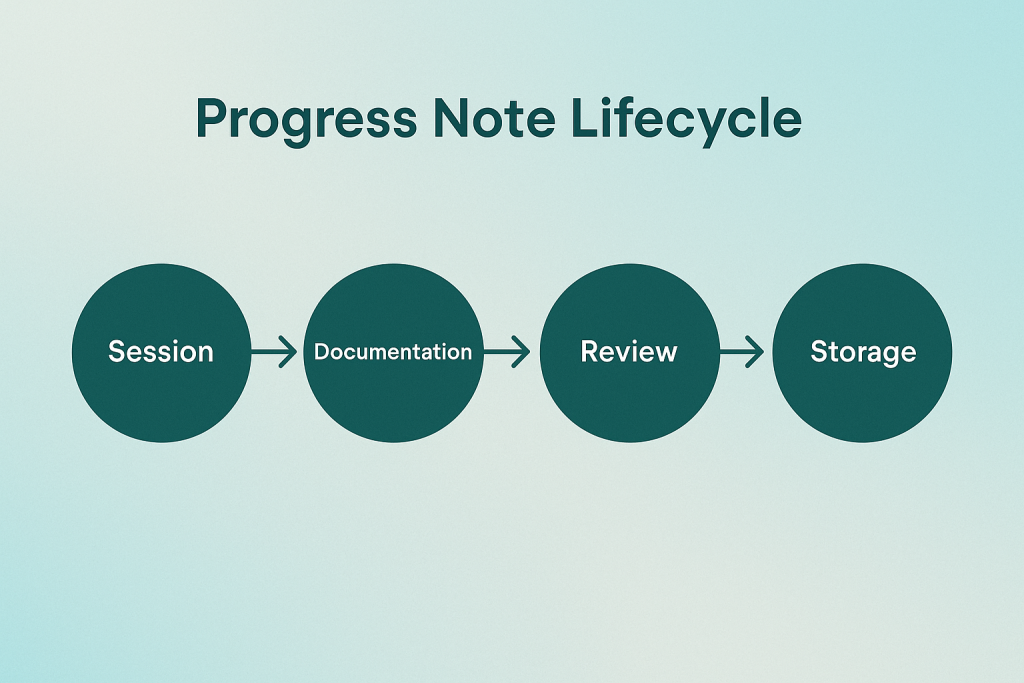
The Progress Note Lifecycle (timeline)
The simplest way to stay current is a two-step habit: capture a brief “quick note” right after session, then finalize once a day. This avoids late-night catch-up and keeps details accurate.

Teams I train block a 20–30 minute “finalize” window once per day. It’s short enough to be realistic and long enough to keep charts audit-ready.
Real progress note examples you can adapt
Use these samples as patterns. Tailor the voice to your practice and client population. The key is specificity: show what changed, what you did, and what happens next.
Progress note — Individual therapy (anxiety)
Date/Modality: 2025-03-18, Telehealth. Session length: 53 min. Present Focus: Pt reports heightened worry before presentations; sleep fragmented (awake 3–4am). Interventions: Cognitive restructuring on “what-if” chains; 4-7-8 breathing practice; psychoeducation on sleep window. Response: Pt able to identify 2 common worry distortions; breathing reduced SUDS from 6→4 within session. Clinical Impression: GAD, moderate. Symptoms partially responsive to skills; performance triggers remain. Plan: Assign 5-min breathing 2x/day; prepare one realistic “safety thought” card; track awakenings; next in 1 week.
Progress note — Medication management (depression + anxiety)
Date/Modality: 2025-04-01, Clinic. Session length: 30 min. Present Focus: Mood improved; energy fair; anxiety spikes around deadlines; early morning awakening persists. Interventions: Med review of Sertraline 50mg; side effects neg; reinforced adherence; introduced PMR handout. Response: Pt reports fewer low-mood days; PHQ-9 13→9; GAD-7 12→11; agreeable to skills use. Clinical Impression: MDD, recurrent, mild; GAD—improving. Partial response to SSRI; skills supporting functional gains. Plan: Continue Sertraline 50mg; practice PMR nightly x10 min; therapist to focus on performance anxiety; follow-up in 3 weeks.
Progress note — Group therapy (interpersonal skills)
Date/Modality: 2025-03-25, In-person. Session length: 75 min. Present Focus: Themes—boundary setting and people-pleasing. Two members shared successes with saying “no.” Interventions: Role-play “I” statements; feedback round on nonverbal signals; homework debrief. Response: Members showed improved assertiveness; 4/6 attempted role-play; one member practiced reflective listening. Clinical Impression: Group progressing in skill generalization; peer feedback strengthening motivation. Plan: Homework—one “I” statement in real context; note outcome; next group in 1 week; individual sessions address barriers.
If you prefer to frame each entry in SOAP, map the same content to Subjective, Objective, Assessment, and Plan. See our companion guide: How to Write SOAP Notes.
Time-savers, strategies, and common pitfalls
- Do the “quick note” while details are fresh: 3–6 sentences right after session. Perfection is for the finalize block.
- Write for handoff: Imagine a colleague reading your note tomorrow. Would they know what to do next?
- Pair with a living treatment plan: When you change tactics, add a line in the plan and state why. See how to write a mental health treatment plan.
- Field-test your phrasing: Replace vague text (“did CBT”) with what you actually did (“guided cognitive restructuring around catastrophizing”).
- Track outcomes simply: Trend PHQ-9/GAD-7 or functional markers (e.g., school attendance, sleep duration).
- Document risk precisely: Quotes, context, protective factors, and safety actions — in the same paragraph.
- Use short templates, not boilerplate: Start from a tight pattern then personalize. Boilerplate invites denials.
- Schedule a daily finalize window: 20–30 minutes is enough to polish, file, and keep audits painless.
- Note constraints: Late starts, tech issues, or environment limits belong in context (it explains outliers).
- Mind privacy: Avoid extraneous details that don’t advance care or necessity.
Personal lesson: my notes got faster when I stopped “writing everything that happened” and started “writing the few things that change care.” When in doubt, ask: Does this sentence help another clinician make a decision?
Key takeaways
- Every progress note should show change, intervention, and next steps.
- A two-step habit (quick note + daily finalize) keeps charts current without burnout.
- Specific interventions and clear clinical impressions strengthen medical necessity.
- Use the same outcome markers payers recognize and trend them over time.
- Keep your progress notes aligned with a living treatment plan and session-level SOAP entries.
Frequently asked questions
1) How long should a progress note be?
2) How soon should I write it?
3) Do I need standardized measures every time?
4) How detailed should the intervention be?
5) Where do I document risk?
6) Is copying prior notes acceptable?
7) Progress note vs. SOAP note?
8) How do progress notes relate to treatment plans?
9) What about telehealth specifics?
10) Any tips for busy days?
Author & Reviewer

TherapyDial Editorial Team
Clinically reviewed by licensed therapists to ensure accuracy, clarity, and compliance.