How to Write SOAP Notes — A Practical Clinician’s Guide
Clear, insurance-ready documentation that protects your practice and respects your time. Below you’ll find the exact SOAP structure I teach new clinicians, example notes you can adapt, and a clean workflow timeline to help you finish faster without sacrificing clinical nuance.

Progress notes don’t have to be a grind. With a reliable SOAP structure, you can document efficiently, stay insurance-ready, and still capture the “why” behind your work. If you’re building goals alongside your notes, see our companion guide How to Write a Mental Health Treatment Plan for a step-by-step approach to goals, objectives, and interventions.
What is a SOAP note?
SOAP stands for Subjective, Objective, Assessment, Plan. It’s a simple structure that helps other providers, payers, and auditors quickly understand the session, your reasoning, and the next steps. Done well, it’s concise and powerful — a consistent way to turn the session’s story into clinical documentation.
The goal isn’t verbosity; it’s clarity. When you learn how-to-write-soap-notes with purpose, you’ll protect your schedule and your chart.
Why SOAP works for compliance & continuity
Payers expect to see the client’s report (S), observable findings (O), your professional interpretation (A), and the plan (P). SOAP mirrors these requirements. It also helps colleagues orient quickly when covering your caseload — a critical continuity-of-care benefit.
If you’re also setting longer-term goals or adjusting care pathways, pair your SOAP notes with a living treatment plan: How to Write a Mental Health Treatment Plan.
How to write SOAP notes — step-by-step
Subjective
Capture the client’s own report — mood, symptoms, stressors, and relevant quotes. Keep it tied to diagnosis and treatment. In practice, I find one short quote per session adds authenticity and reduces denials (e.g., “I wake up anxious and can’t get back to sleep.”).
- Summarize the presenting concern and changes since last session.
- Document relevant self-report scales or screening items, if used.
- Avoid interpretation here — that belongs in Assessment.
Objective
Record what you observe and measure: affect, appearance, speech, behavior, and any scores (PHQ-9, GAD-7). Include risk indicators and modality (e.g., telehealth) if relevant to billing and care.
- Include specific observations (e.g., “tearful, limited eye contact”).
- Record scores and vitals/side effects if in scope.
- Note barriers (e.g., tech issues) that affected care delivery.
Assessment
Synthesize S + O into your clinical impression: diagnosis, progress, risk, and rationale. Be explicit about why the diagnosis fits (“MDD, single episode, moderate — anhedonia, low mood most days, PHQ-9 = 14”).
When you notice the treatment trajectory is shifting, update the plan document too. If you need a refresher on structuring goals and objectives, see How to Write a Mental Health Treatment Plan.
Plan
Spell out what happens next: interventions, frequency, homework, referrals, care coordination, and risk/safety steps. Specificity matters for medical necessity (e.g., “Weekly CBT skills + sleep hygiene; safety plan reviewed; med consult 4/1/2025.”).
- Include follow-up timeframes (“next session in 1 week”).
- Note provider coordination and rationale for changes.
- Align with the active treatment plan where appropriate.
SOAP examples you can adapt
These examples balance brevity and specificity so they remain clinically useful and insurance-ready. Adapt the phrasing to your voice and the session’s content.
SOAP note — Individual therapy
Client: Connor Client | DOB: 02/02/1992
Date: 7/10/2023 | Time: 1:33–2:30pm (57min) | Location: Office
S: "Feeling brighter" since last session; used coping skills daily; engaged at family event; still difficulty falling asleep.
O: Affect brighter; improved eye contact; engaged; PHQ-9 = 8; no SI/HI; well groomed.
A: MDD, single episode, moderate — improving; residual insomnia.
P: Continue weekly sessions; sleep hygiene + relaxation; behavioral activation homework; monitor mood and sleep; next appt 7/17/2023.
SOAP note — Medication management
Client: Michael Martinez | DOB: 11/15/1988
Date: 3/18/2025 | Time: 2:15–3:12pm (57min) | Location: Clinic
S: Anxiety about upcoming presentation; "Sertraline helps mood but not performance anxiety."
O: Alert, oriented x4; PHQ-9 = 9 (down from 13); GAD-7 = 14 (up from 12); pressured speech discussing work; denies SI/HI.
A: GAD with performance-related exacerbation; partial response to antidepressant.
P: Continue Sertraline 50mg; add PMR + cognitive restructuring; med follow-up 4/1/2025; weekly therapy; maintain anxiety log.
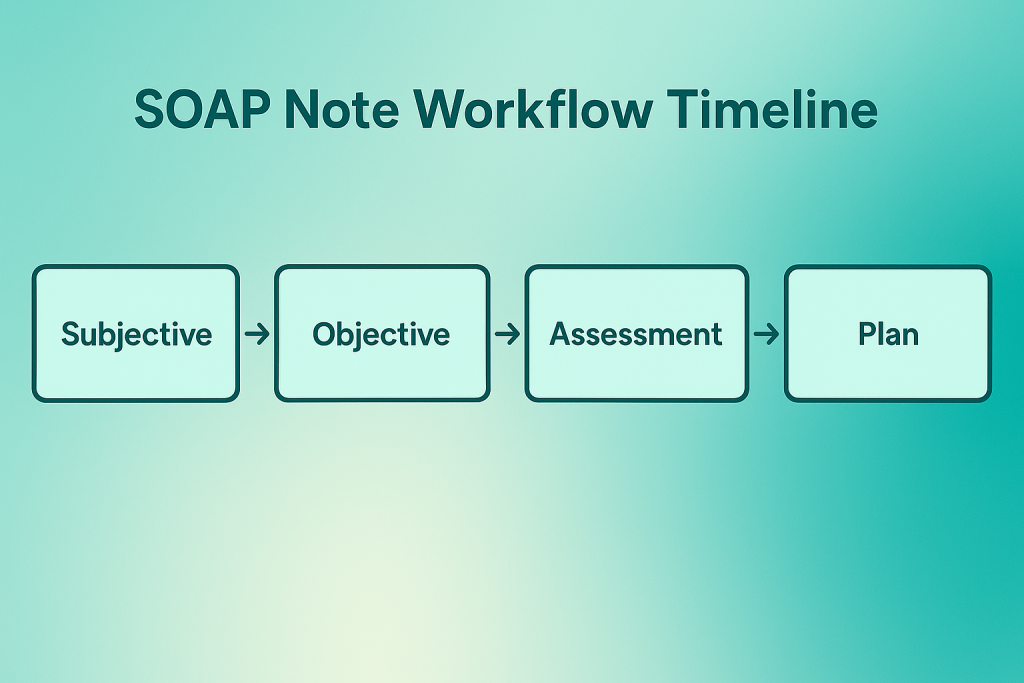
SOAP workflow timeline (visual)
A simple cadence keeps documentation timely: a quick note immediately after session, then a brief end-of-day finalize. This avoids backlogs and improves accuracy.
I coach teams to calendar a single 20–30 minute “finalize block” daily. It’s short enough to be sustainable and long enough to keep charts audit-ready.
Templates & shortcuts
S: Increased anxiety this week; sleep ~5h/night. O: Affect anxious; GAD-7 = 12; no SI/HI; engaged. A: GAD, moderate — worsened with work stress. P: Teach paced breathing; weekly therapy; sleep routine; track anxiety episodes.
S: Mood better; performance anxiety persists. O: PHQ-9 13→9; GAD-7 12→14; no SI; vitals WNL. A: Partial antidepressant response; performance triggers present. P: Continue med; add PMR + cog restructuring; review SEs next appt.
S: Themes: isolation, boundary difficulty; members report mixed success with homework. O: Active participation; peer feedback observed; affect modulation attempts. A: Improving interpersonal skill use; several members show increased insight. P: Continue role-play; assign boundary-setting homework; monitor risk individually.
Practical tips that save time (and audits)
- Quick note first, polish later: 2–3 lines immediately post-session; finalize once daily.
- Be specific, not verbose: Keep every sentence tied to diagnosis, progress, or plan.
- Add one direct quote: Authenticates the session and supports medical necessity.
- Track outcomes: Use the same measures payers recognize (PHQ-9, GAD-7); trend them.
- Reuse short templates wisely: Start from a tight pattern, then personalize.
- Document risk precisely: Record statements, context, and safety steps in the chart.
- Schedule a daily “finalize block”: Prevents backlog and improves quality control.
Personal note: when I adopted a “quick note + daily finalize” cadence, my average documentation time dropped by half — and chart quality improved because I wasn’t relying on memory at 9pm.
Related Reading
Building goals and measurable outcomes? Pair your SOAP notes with a strong plan: How to Write a Mental Health Treatment Plan.