Depression ICD-10 Codes: F32 & F33 Explained
A practical, visual reference for clinicians: the most-used codes, how to pick the right specificity, ICD vs DSM tips, exclusions to watch, and real-world examples for cleaner charts and fewer denials.
Quick context
How ICD-10 organizes depressive disorders
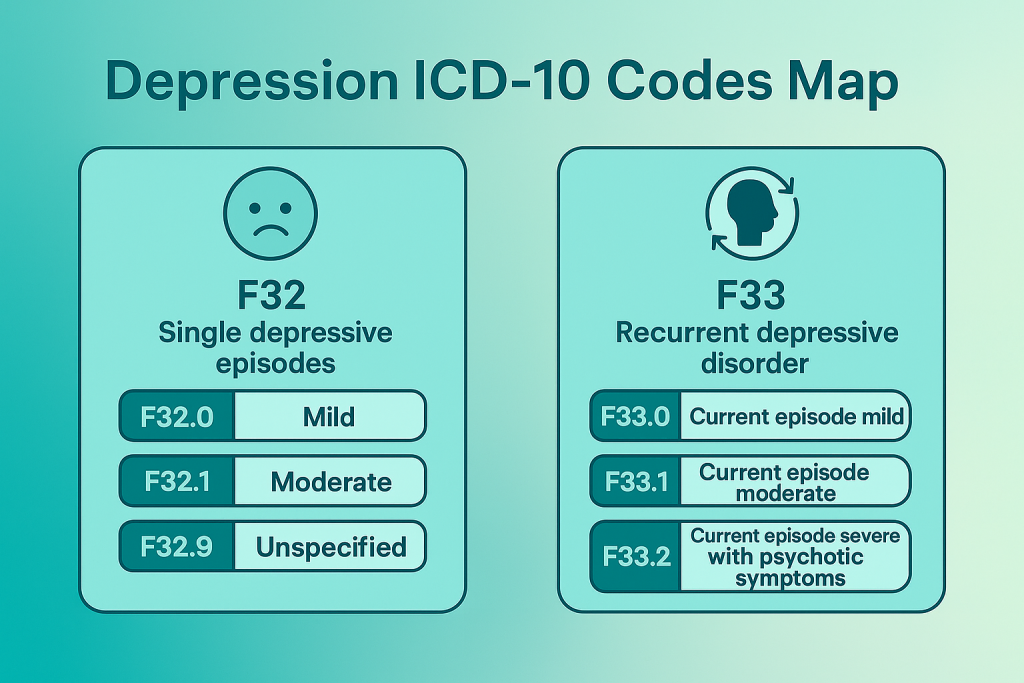
ICD-10 groups depressive disorders into two major families: F32 (single depressive episode) and F33 (recurrent depressive disorder). Severity is specified as mild, moderate, or severe, with an option to indicate with or without psychotic symptoms for severe episodes.
F32 — Single depressive episodes
Use F32 codes when the current presentation is a first-time or single episode. The core symptom cluster includes lowered mood, reduced energy/activity, anhedonia, diminished concentration, sleep/appetite disturbance, and reduced self-esteem; severity is determined by the number and impact of symptoms.
F32.0 Mild depressive episode
- Typically 2–3 core symptoms with distress but preserved basic functioning.
- Document functional examples (e.g., reduced productivity, social withdrawal).
F32.1 Moderate depressive episode
- Four or more symptoms with significant difficulty maintaining ordinary activities.
- Track symptom measures (e.g., PHQ-9) to show medical necessity.
F32.2 Severe without psychotic symptoms
- Marked impairment, often with psychomotor changes, diurnal variation, guilt/worthlessness.
- No delusions or hallucinations present.
F32.3 Severe with psychotic symptoms
- Severe episode with mood-congruent or incongruent psychotic features.
- Coordinate with medication management/psychiatry; safety plan and risk documentation required.
F32.9 Depressive episode, unspecified
- Use temporarily when details are insufficient; refine once data are complete.
- Include a plan (e.g., collateral, labs, rating scales, follow-up) to increase specificity.
F33 — Recurrent depressive disorder
Use F33 codes when there are repeated episodes of depression (with no independent history of mania). Code severity for the current episode; severe episodes can be specified as with/without psychotic symptoms.
F33.0 Recurrent — current episode mild
Meets mild threshold; previous episodes documented. No manic history. Capture residual symptoms and functioning between episodes.
F33.1 Recurrent — current episode moderate
Four or more symptoms and notable functional interference. Include longitudinal context and response to prior treatments.
F33.2 Recurrent — current episode severe without psychosis
Severe symptom burden with no psychotic features. Risk assessment, level-of-care justification, and safety planning should be explicit.
F33.3 Recurrent — current episode severe with psychosis
Psychotic features present. Coordinate with psychiatry; document rationale for medication, monitoring, and care transitions if needed.
F33.9 Recurrent depressive disorder, unspecified
Temporary placeholder when episode severity or psychotic status is unclear. Add a plan to obtain specificity (e.g., collateral, repeat measures).
ICD vs DSM — quick comparison (cards)
Single Depressive Episode
Use when this is the first or only episode documented. Code current severity (mild / moderate / severe ± psychosis).
Recurrent Depressive Disorder
Use when there are repeated episodes without manic history. Code the severity of the current episode.
Criteria & Specifiers
DSM-5 provides the diagnostic criteria (duration, symptoms, impairment) and specifiers (e.g., anxious distress, melancholic).
Exclusions & coding cautions
Real-world coding examples
PHQ-9 = 14, anhedonia, low mood, fatigue, morning worsening; no psychosis; no manic history. ICD-10: F32.1 (Moderate) Chart cue: document functional impacts and sleep/appetite changes.
Multiple prior episodes; current PHQ-9 = 21, psychomotor retardation; no delusions/hallucinations. ICD-10: F33.2 (Severe, no psychosis) Chart cue: include risk assessment and care plan (e.g., med review, safety plan).
Mood-congruent delusions; impaired functioning; prior similar episode. ICD-10: F33.3 (Severe with psychosis) Chart cue: coordinate with psychiatry; document rationale for LOC and monitoring.
Depression coding workflow (at a glance)
Pair the chosen ICD code with DSM-5 criteria justification, functional examples, measures (PHQ-9), and a clear treatment plan.
Related TherapyDial guides
Need help standardizing documentation?
We help teams align intake, progress notes, treatment planning, and discharge—without adding admin drag.
Talk to a Practice Consultant