Emotions shape how we see, decide, and connect. When feelings are too painful or risky to face, the mind sometimes pushes them out of awareness. This protective reflex—emotional repression—can quiet distress in the short term but often leaves ripples in the body and mind. This guide explains what repression is (and how it differs from suppression), why it happens, how to spot the signs, and practical ways to work through it—on your own and with a therapist.
Key Takeaways
- Repression is the unconscious blocking of painful emotions and memories; suppression is a conscious effort to set feelings aside. If you also feel “emotion blind,” see our guides on alexithymia and relationship tips.
- Repressed emotions can surface as physical symptoms (tension, headaches, GI upset), anxiety, low mood, avoidance, or memory gaps. For a gentle skills primer, try journaling out of numbness.
- Gentle, repeatable skills—journaling, mindfulness, movement, self-compassion, and creative outlets—help feelings become tolerable and workable. CBT tools can help challenge stuck thinking (see DIY CBT exercises).
- When distress lingers or daily life narrows, evidence-based therapies (e.g., CBT; trauma-focused care like TF-CBT/EMDR) are effective and safe. Read our overviews of CBT therapy and EMDR for childhood trauma.
- Recovery is a process: learn the signals, pace the work, build support, and partner with a clinician when you’re ready. If sleep is a bottleneck, see CBT-I sleep reset or soothing ASMR sleep triggers.
What is Emotional Repression?
In classical psychology, repression is a defense mechanism where the mind unconsciously keeps distressing feelings, impulses, or memories out of awareness to reduce anxiety. The person isn’t choosing this; it happens automatically as a form of self-protection. By contrast, suppression is when you knowingly set something aside (“I’ll think about this after work”).
Plain-English check: If you’re choosing to park a feeling for later, that’s suppression. If it never seems to “arrive” in consciousness—or shows up indirectly as tension, numbness, or avoidance—that may be repression. If “no words for feelings” is your norm, learn about alexithymia.
Repression can follow trauma, long-term stress, invalidating environments, or family/cultural messages like “Don’t cry” or “Be strong.” It can provide short-term relief. Over time, though, the sealed-off emotion still “leaks” through the body, mood, and relationships.
Repression vs. Suppression (Quick Comparison)
| Feature | Repression | Suppression |
|---|---|---|
| Conscious control? | Unconscious | Conscious, deliberate |
| Short-term effect | Reduces anxiety outside awareness | Creates space to function or self-regulate |
| Long-term risk | Unprocessed feelings surface indirectly (somatic tension, mood symptoms) | If overused, emotions “bottle up” and spill over later |
| Helpful use case | Protective reflex in overwhelming moments | Time-boxing feelings (e.g., “I’ll journal tonight”) |
A nuanced point: thoughtful, time-limited suppression can be a useful skill (e.g., during a work meeting)—as long as those feelings get returned to and processed later. Try these journal prompts for numbness.
Why Does Repression Happen?
- Trauma or overwhelming events: the nervous system prioritizes survival; the mind may “wall off” experience to function. If trauma is relevant, see EMDR explained and PTSD treatment in NYC.
- Learning & environment: if big feelings are shamed or ignored, you may learn to push them down to keep relationships safe.
- Skill gaps: without tools for naming, tolerating, and soothing emotions, avoidance feels like the only option. Build skills with DIY CBT exercises.
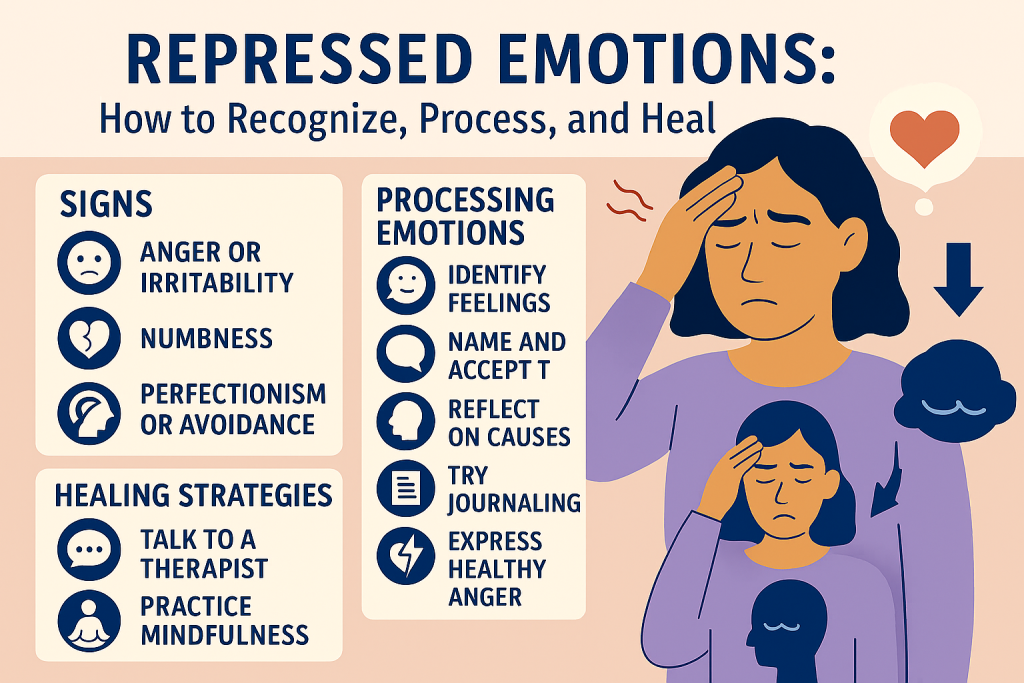
Common Signs of Repression (and Over-Suppression)
Physical signals without a clear medical cause
Muscle tension, headaches, stomach upset, chest tightness, fatigue, or non-specific aches can reflect stress load and held emotion. Always rule out medical issues with a clinician; when tests are normal, look at stress patterns and coping habits. For day-to-day stress tools, see our science-backed stress guide.
Emotional patterns
Numbness, “I don’t know what I feel,” irritability, sudden spikes in anxiety, or a flat mood. If you resonate with feeling “emotion blind,” skim alexithymia basics.
Memory + avoidance
Difficulty recalling chunks of stressful periods, steering clear of places, topics, or people that stir feelings, or getting “small” in life to avoid triggers. For nightmare-specific support, try grounding to wake up calm.
Relationship effects
Feeling distant, snapping at loved ones, or needing lots of control and predictability to feel safe. If your partner says you seem “hard to read,” these 3 relationship strategies can help.
If these patterns persist or intensify, consult a mental health professional. Therapy offers a paced, evidence-based way to work safely with what emerges.
How Repressed Feelings Affect Body & Mind
Chronic, unprocessed stress doesn’t just feel bad; over time, it can feed elevated blood pressure, sleep disruption, changes in appetite, and mood symptoms. That’s why “feeling better” and “getting physically healthier” often travel together.
Good news: small, consistent habits do change the stress system. Sleep regularity, movement, social connection, and simple breathwork can lower baseline arousal—and make emotional work feel more doable.
For further reading on stress and health, see overviews from NIMH, NCCIH, and Harvard Health.
Step-by-Step: Gentle, Practical Ways to Work with Repressed Emotions
1) Micro-journaling (5–10 minutes)
- Prompt: “Right now I notice… in my body / emotions / thoughts.” Use these journal prompts for emotional numbness.
- Containment: end with: “One thing I’ll do to care for myself after writing is…”
- Boundaries: if you feel activated, stop, ground (see below), and consider bringing this to therapy.
2) Mindfulness that meets you where you are
- Label + allow: name one feeling (“sad,” “angry,” “scared”) and one sensation (“tight chest,” “warm face”).
- Anchor: feel your feet or inhale for 4, exhale for 6 for one minute.
- Practice dose: 3 minutes is enough to start; daily repetition > long sessions.
3) Creative outlets
Free-form art, music, or dance helps emotions move without words. No talent required—the goal is expression and relief.
4) Movement & nervous-system resets
- Brisk walk, light jog, yoga, or paced breathing after stressful interactions.
- Pair movement with a short reflection: “What was I feeling right before I needed this?”
5) Safe social connection
Reach out to a trusted person and share a small, specific piece (e.g., “I’ve been feeling tight-chested after work; could we take a 10-minute walk?”). Co-regulation calms the nervous system and makes feelings more thinkable.
6) When to add therapy
Consider professional support if: symptoms persist for weeks, you feel stuck or numb, daily life narrows (avoiding, isolating), or if trauma is in the picture. Therapy offers pacing, skills, and a safer container. Compare approaches in our CBT overview and trauma resources (EMDR, PTSD treatment in NYC).
From Recognition to Recovery: A Simple Timeline
Notice & Name
“I’m tense and snappy after difficult emails.” One emotion + one sensation.
Ground & Soothe
60–120 seconds of slow breathing; feel the chair and your feet.
Express
Micro-journal, voice note, or draw for 5 minutes. Close with one doable care action.
Make Meaning
Ask, “What does this feeling want me to protect or change?”
Get Support
Share one specific line with a trusted person or therapist; schedule care.
Practice
Repeat small steps most days. Track shifts in tension, sleep, and mood.
Therapy Options that Help with Repressed Emotions
CBT (Cognitive Behavioral Therapy)
CBT helps you map how thoughts, feelings, and behaviors interact. You learn to identify avoid-feel-numb cycles and replace them with skills that reduce distress and open room for values-based action. Many people notice improved mood and less anxiety within weeks when sessions are paired with between-session practice. A quick refresher on reframing is here: challenge cognitive distortions.
Trauma-focused work (TF-CBT, EMDR)
When trauma is relevant, these approaches help you safely process what happened, update beliefs (“It was my fault” → “I did what I could to survive”), and reduce triggers. Therapy is collaborative and paced; the aim is integration, not re-living. Learn more via EMDR guide and PTSD care options.
Emotion skills inside therapy
- Psychoeducation: normalizing the body’s stress responses.
- Skills training: grounding, distress tolerance, and emotional labeling. If labeling is tough, see 3 ways to build awareness.
- Gradual exposure: stepping toward avoided feelings/situations at a tolerable pace.
- Meaning-making: rebuilding narratives that support connection and agency.
About “recovered memories”: memory is complex and suggestible. Ethical therapy doesn’t force memories or assume they must be present or absent. The goal is present-day safety and functioning, with care around the limits of recall. For nighttime distress, practice these nightmare grounding techniques.
Real-Life Mini-Examples (Names Changed)
“The Headache After Every Meeting”
Taylor noticed a pounding headache after weekly check-ins. A 7-minute routine (2 minutes breathing, 3 minutes journaling, 2 minutes stretching) reduced headaches within three weeks. In CBT, they discovered the core emotion wasn’t “anger” but fear of criticism; practicing boundary scripts (“Let me circle back once I review the data”) lowered anticipatory anxiety.
“The Nightmares”
Sam began trauma-focused therapy. Early work emphasized safety, sleep routines, and body-based grounding before processing memories. Nightmares decreased as Sam felt more choice in attention and learned to exit flashbacks with 5-senses grounding (see waking up calm).
“The Numbness”
Jordan felt flat for months. With gentle behavioral activation (10-minute walks, call one friend), emotion labeling, and values exercises, they noticed more moments of interest and warmth. Therapy targeted self-criticism, which had been silencing grief. For daily prompts, try this journaling routine.
A Week of Strategies You Can Repeat
| Day | Focus | Micro-Practice (10–15 min) |
|---|---|---|
| Mon | Name & Notice | Body scan from feet to face; write 5 sensations + 1 emotion word. If labeling is tough, browse alexithymia basics. |
| Tue | Breath & Ground | 4-6 breathing for 5 minutes; note any shift (tension, temperature, urge). For nighttime anxiety, see CBT-I sleep reset. |
| Wed | Express | Journaling sprint: “If my body could talk, it would say…” Use these prompts. |
| Thu | Connect | Text a friend to walk or talk; share one specific feeling. If social fear spikes, try 5 CBT techniques at home. |
| Fri | Meaning | Values check-in: “What mattered this week?” Plan one small, aligned action. When worries lean global, explore eco-anxiety techniques. |
| Sat | Create | 10-minute drawing or music session. No judgment, only flow. |
| Sun | Review & Plan | Two lines: “What helped” and “What I’ll try next week.” For cognitive tune-ups, practice CBT distortion challenges. |
FAQs
What’s an example of repression vs. suppression?
Repression: You can’t recall parts of a stressful period and feel inexplicably tense around certain topics. Suppression: You choose to shelve a feeling (“I’ll revisit after dinner”), then return to process it with journaling or a walk—use our journaling guide.
Is it bad to suppress emotions?
Brief, intentional suppression can be useful (e.g., pausing tears in a meeting). The key is coming back to the feeling later. Chronic avoidance tends to raise stress and narrow life. If you’re unsure where to start, try CBT basics.
How do I know if I need therapy?
If symptoms persist for weeks, interfere with sleep/work/relationships, or if trauma is part of your history, therapy is recommended. A clinician will pace the work and teach skills for safety and regulation. Learn how we work at TherapyDial.
Can therapy “recover” repressed memories?
Memory is malleable. Ethical therapists avoid pressuring recall or making assumptions. The focus is building present-day safety, functioning, and meaning; if memories emerge, they’re handled carefully alongside corroborating context. For nighttime symptoms, see nightmare grounding.
Which therapies help?
CBT can reduce anxiety/depression and avoidance patterns. For trauma, trauma-focused CBT or EMDR are common options. Explore CBT therapy and EMDR for childhood trauma.
When to Seek Support Immediately
If you’re thinking about harming yourself or feel unable to stay safe, seek help now. Call your local emergency number or visit the nearest ER/ED. In the U.S., call or text 988 for the Suicide & Crisis Lifeline.