Evidence-based EMDR care in New York City—online and in person. Below, you’ll find a plain-English explainer of how EMDR works, who it helps, realistic timelines (weekly vs. intensives), transparent costs & access, and a comparison with CBT/CPT/PE so you can choose what fits. (Endorsements by major bodies are summarized with links.)
Key Takeaways
- EMDR is an evidence-based trauma therapy used by PTSD programs worldwide (endorsed or recommended in guidance from APA, WHO, and the VA/DoD). See sources linked in this page.
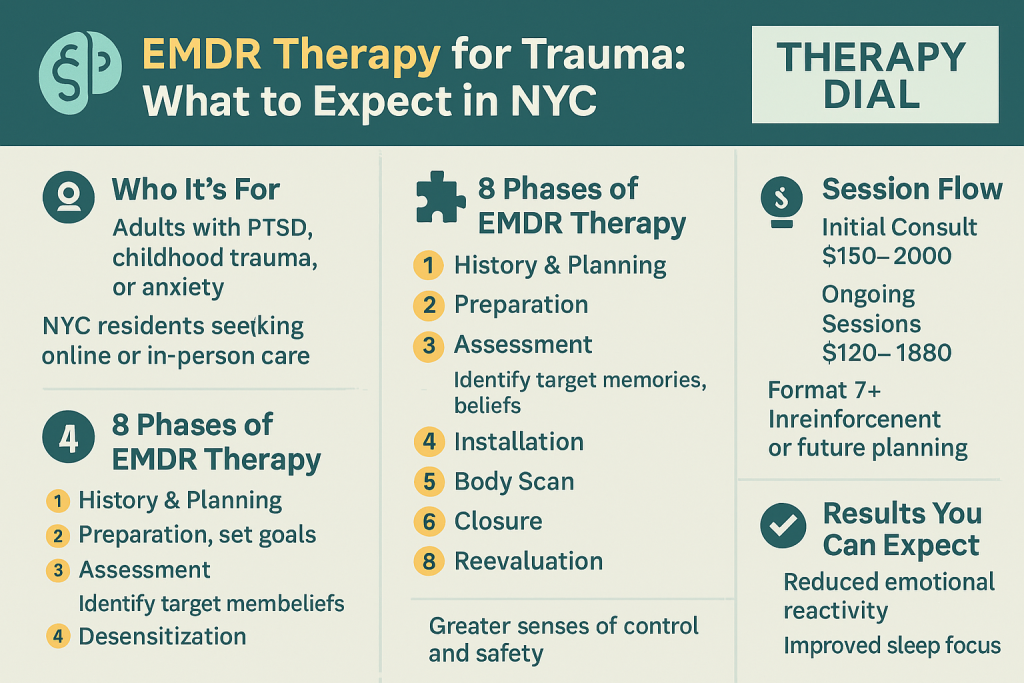
- It’s structured (8 phases) and can be delivered in person or via secure telehealth with simple tools (eye movements, taps, tones).
- Good fits: PTSD and complex trauma, medical trauma, grief, and specific phobias; many clients report sleep/stress improvements as symptoms resolve.
- Costs & access: NYC has private-practice options and low-fee programs; out-of-network reimbursement may offset fees.
- Not sure EMDR is your best first step? Compare EMDR vs. CPT/PE/TF-CBT in the table below, or start with a quick consult.
What Is EMDR (in Two Paragraphs)
Eye Movement Desensitization and Reprocessing is a trauma-focused psychotherapy that helps the brain reprocess distressing memories using bilateral stimulation (e.g., guided eye movements, taps, or tones). Multiple national bodies include EMDR among recommended PTSD treatments for adults, reflecting a substantial evidence base. APA PTSD Guideline (2025), WHO trauma care guidance, and the VA/DoD PTSD resources describe EMDR among effective trauma therapies.
EMDR follows an eight-phase protocol (history, preparation, assessment, desensitization, installation, body scan, closure, re-evaluation). Sessions typically run 60–90 minutes; weekly care is common, and some clinics offer intensives (condensed schedules). See EMDRIA’s explainer on the phases and credentials, and APA’s overview for more detail.
- Phases overview: EMDRIA: The Eight Phases • APA topic page
Is EMDR Right for Me? (Quick Self-Check)
- Recent single event (car crash, assault, medical emergency) and ongoing intrusive memories or hyperarousal.
- Complex / developmental trauma with long-standing triggers in relationships or self-worth.
- Medical trauma (procedures, ICU) with avoidance of care settings.
- Sleep disturbance, nightmares, or startle response that won’t settle.
Not sure? If stress and insomnia are your main barriers, you might blend EMDR with sleep skills. See our CBT-I 14-day reset and ASMR sleep triggers.
Who EMDR Helps (NYC Examples)
- PTSD & Complex PTSD from assault, abuse, accidents, disasters.
- Medical trauma (procedures, ICU stays, chronic illness flares).
- Grief and loss, specific phobias, performance blocks.
- When sleep is disrupted: integrate EMDR with CBT-I and soothing tools like ASMR.
See also our PTSD primers and local resources: PTSD treatment in NYC • Nightmare grounding.
How EMDR Works: The 8 Phases (Plain English)
- History & plan: map symptoms, strengths, targets, and safety.
- Preparation: teach grounding and set expectations.
- Assessment: identify target memory and beliefs; rate distress.
- Desensitization: bilateral stimulation while noticing what arises.
- Installation: strengthen adaptive beliefs.
- Body scan: check for residual tension; process if needed.
- Closure: return to present; aftercare plan.
- Re-evaluation: check changes and next targets.
Phase names per EMDRIA & APA summaries. Learn more at EMDRIA and APA.
EMDR vs. CPT, PE, and TF-CBT (Which Fits Your Life?)
| Therapy | How it works | Typical course | Best fit / Pros | Considerations | Guideline notes |
|---|---|---|---|---|---|
| EMDR | Bilateral stimulation while processing memories; 8 structured phases (AIP model). | Weekly 60–90m; 6–12+ sessions; intensives possible. | Less homework than CPT/PE; effective for single-event and complex presentations; can combine with sleep skills. | Emotional activation is normal; needs prep skills; choose trained/EMDRIA-certified clinicians when possible. | Included among recommended PTSD therapies by APA/WHO; strong support across VA/DoD resources. |
| CPT | Cognitive Processing Therapy: identify and shift stuck trauma beliefs. | ~12 sessions, weekly. | Great for meaning-making and belief change; clear homework structure. | More written work; exposure elements for some clients. | Recommended in APA/VA-DoD guidelines. |
| PE | Prolonged Exposure: imaginal + in-vivo exposure reduces avoidance. | 8–15 sessions; intensive options exist. | Strong evidence; direct fear learning updates. | High activation; significant homework and between-session practice. | Recommended in APA/VA-DoD guidelines. |
| TF-CBT | Skills + trauma processing; often used for youth but helpful for adults too. | 12–20 sessions; flexible skills first, processing later. | Great on safety/skills; family-involved variants. | Processing pacing varies; may be longer with complex trauma. | Recognized across major guidance bodies. |
Cost, Insurance & Access in NYC (Radical Transparency)
- Private practice: EMDR sessions in NYC often range $200–$350+; some publish rates (e.g., Soho Integrative EMDR lists $275/45m & $350/60m).
- Low-fee options: The NIP Treatment Center offers EMDR on a reduced-fee sliding scale (in-person and telehealth).
- Hospital-affiliated programs: See NYU Langone’s Trauma Program for broader trauma services.
- Out-of-network reimbursement: If you have PPO insurance, OON benefits may cover a portion; ask for a superbill.
Tip: Combine EMDR with practical skills between sessions—our DIY CBT distortion drills and science-backed stress guide can speed progress.
What to Expect: From Inquiry to Session 6
Inquiry & Fit
Brief consult, goals, scheduling, and coverage. Safety planning if needed.
Assessment
History, targets, and baseline measures; choose weekly vs. intensive format.
Preparation
Grounding, sleep & stress tools, expectation setting; practice bilateral cues.
First reprocessing
Start with a contained target; aftercare routine (hydration, journaling, rest).
Weeks 3–4
Expand targets; track shifts in distress, sleep, triggers; adjust pacing.
Weeks 5–6+
Generalize gains; plan maintenance skills and relapse-prevention cues.
Common experiences include brief fatigue or vivid dreams—your therapist will provide aftercare and pacing. See general VA/DoD EMDR essentials for more context.
Specialized Tracks
- Complex PTSD: attachment-aware pacing, parts-informed work, skills first; then targeted reprocessing.
- Medical Trauma: stepwise exposure to medical cues + EMDR for procedures or ICU memories.
- Insomnia & Hyperarousal: EMDR + CBT-I sleep plan and soothing routines like ASMR.
Meet Your NYC EMDR Team
Our clinicians are licensed and EMDR-trained; several hold EMDRIA Certified Therapist credentials (a voluntary, advanced pathway beyond basic EMDR training). Learn what “EMDR-trained” vs. “EMDRIA-certified” means at EMDRIA.
FAQs
Is EMDR endorsed by major health organizations?
Yes. EMDR appears among recommended PTSD treatments in the APA PTSD Guideline (2025) and in guidance from the WHO. The VA/DoD PTSD resources also include EMDR among effective options for adults.
How many sessions will I need?
Plans vary with history and goals. Many people work within 6–12+ weekly sessions; complex trauma may take longer. Intensives can condense work into a few days. Your clinician will tailor pacing and aftercare.
Can EMDR be done online?
Yes. Many NYC practices offer telehealth EMDR using guided eye movements or tactile/auditory cues. You’ll review privacy and setup during preparation.
What’s the difference between EMDR-trained and EMDRIA-certified?
After completing approved EMDR basic training, a clinician is EMDR-trained. EMDRIA-certified indicates additional consultation and experience beyond training; it’s voluntary but can signal advanced proficiency.
If You Need Help Now
If you’re thinking about harming yourself or feel unable to stay safe, seek help now. In the U.S., call or text 988 (Suicide & Crisis Lifeline) or go to the nearest ER. If outside the U.S., find a local helpline via your national services.