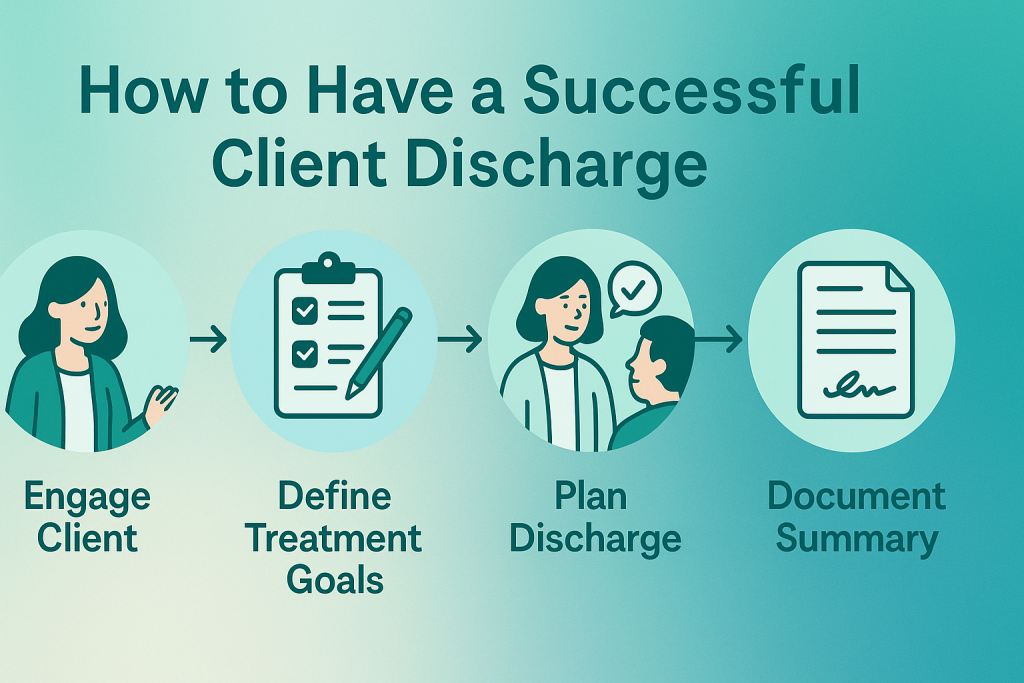
How to Have a Successful Client Discharge (with Discharge Summary Template)
Ending therapy can be just as meaningful as beginning it. A structured discharge process supports client growth, ensures continuity of care, and helps you maintain clinical and ethical standards.
As a clinician, ending therapy is one of the most nuanced moments of care. It’s the point where clinical skill meets human empathy — and documentation meets closure. A client discharge summary isn’t just paperwork; it’s your client’s bridge between what was achieved and what comes next.
What is a discharge summary?
A discharge summary — sometimes called a discharge note — is a concise clinical record summarizing the client’s treatment, progress, and post-therapy recommendations. It’s both a closure document and a professional handoff, ensuring future providers or the client themselves have clarity on progress and next steps.
How to know when to end therapy
Ideally, discharge planning begins with the first session. When you define treatment goals early, you also set the stage for what success and completion look like. Common reasons for discharge include:
- Client has met treatment goals and demonstrates stability
- Client relocates or changes insurance provider
- Therapist leaves position or practice
- Client needs a higher level of care or specialty service
- Lack of engagement or repeated no-shows
Each reason carries different documentation needs, but the principle remains constant: close with clarity and compassion.
How to write a discharge summary
Document the discharge in both your final progress note and a dedicated discharge summary. Write it as soon as possible after the last session — accuracy fades quickly.
Essential information to include
- Client details: demographics, ID, contact info
- Diagnosis: initial and final diagnosis at discharge
- Treatment duration: number of sessions, dates of care
- Goals and progress: what was achieved, what remains
- Interventions used: e.g., CBT, mindfulness, EMDR
- Reason for discharge: completion, referral, or termination
- Post-discharge plan: follow-up, referrals, safety or self-care recommendations
Discharge summary example (template)
| Client Name | Jane Doe |
| Diagnosis | GAD (F41.1), MDD (F32.1) |
| Treatment Dates | Jan 4 – Apr 12, 2025 (12 sessions) |
| Goals Achieved | Reduced daily anxiety; improved sleep; enhanced coping and self-esteem. |
| Reason for Discharge | Goals met — client reports readiness to self-manage. |
| Recommendations | Continue mindfulness practice; follow-up PRN; referral to support group. |
| Therapist Signature | Tanya Therapist, LPC |
Tips for a successful therapy termination
- Reflect on wins: Review progress so clients recognize their growth.
- Create a post-therapy plan: Discuss routines, triggers, and resources for continued well-being.
- Clarify boundaries: Define how (or if) clients can reach out again.
- Honor the relationship: End with empathy; validate the therapeutic journey.
- Bridge the gap: If referring, send release forms and coordinate continuity.
Frequently asked questions
1. When should I discharge a client?
2. How long should a discharge summary be?
3. Is a discharge summary required?
4. Should clients see their discharge note?
5. What if a client drops out abruptly?
Streamline your client care from intake to discharge
Simplify documentation, compliance, and client transitions — so you can focus on care, not paperwork.
Talk to a Practice Consultant