Have you ever felt like your emotions are locked away, just out of reach? You’re not alone. Alexithymia—difficulty identifying and expressing feelings—can make relationships confusing and self-understanding elusive. The good news: with targeted therapies, mindful practice, and small daily habits, most people can learn to read their inner world, name feelings, and express them safely. Start with our primer on the “emotion blindspot” here, then build skills step by step (a gentle journaling approach is here). This comprehensive guide explains the condition, its impacts and causes, how clinicians assess it, and the most effective treatment paths—plus step-by-step plans, real-life examples, and answers to common questions.
Key Takeaways
- Alexithymia means difficulty noticing, identifying, and describing emotions; it is a trait-dimension that can improve with skills and therapy. If relationships are affected, see relationship-focused strategies.
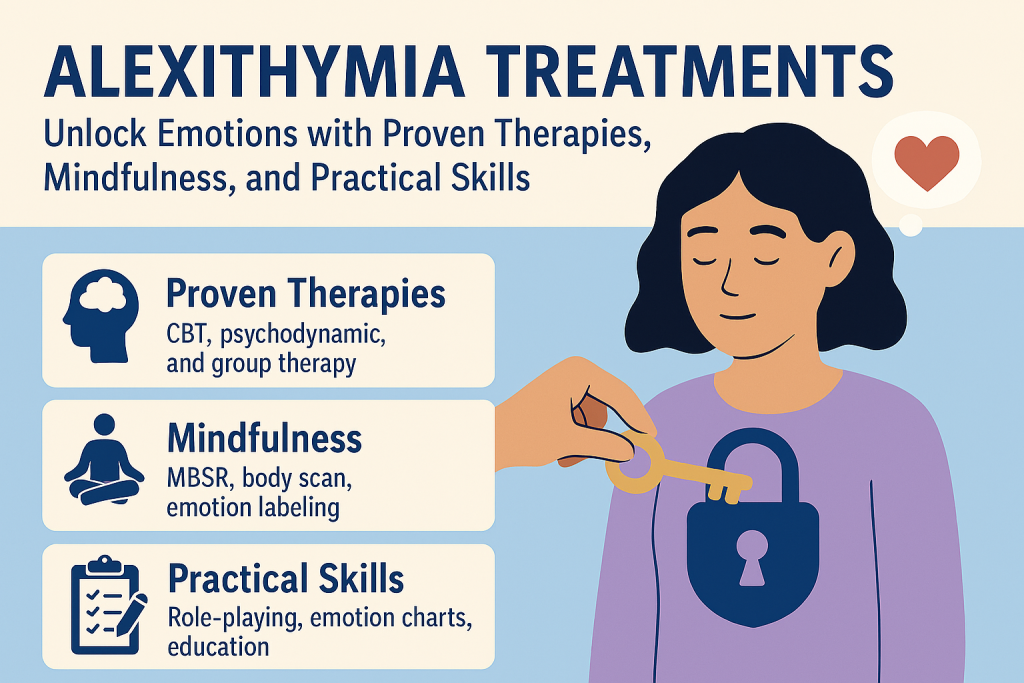
- Effective care blends psychoeducation, CBT or emotion-focused strategies, mindfulness & interoception, and communication practice. A CBT overview is here.
- Assessment may include structured interviews and tools such as the Toronto Alexithymia Scale (TAS-20) alongside clinical judgment.
- Supportive relationships, groups, and consistent lifestyle habits (sleep, movement, nutrition) lower stress and make feeling-skills stick. For sleep trouble, try CBT-I sleep restriction.
- Seek professional help when symptoms persist, relationships suffer, or co-occurring anxiety/depression are present. For stress tactics, see our science-backed stress guide.
Understanding Alexithymia: Definition and Symptoms
The word alexithymia literally means “no words for emotions.” People may notice a muted internal signal (“I know something is off, but I can’t tell what”), difficulty labeling feelings (“good/bad” instead of more precise words), and trouble sharing emotions in conversations. Some experience a flat affect or rely on concrete, practical thinking while avoiding reflective or feeling-language. If you’re unsure whether “emotionless” behavior is alexithymia or something else, compare alexithymia vs. sociopathy.
Common signs include: limited emotional vocabulary, confusion between emotions and bodily sensations, indecision driven by unclear preferences, difficulties recognizing others’ feelings, and somatic complaints (headaches, GI upset) that track stress even when emotions aren’t consciously noticed.
Important: Alexithymia is not a character flaw. It reflects learned patterns, nervous-system sensitivity, and sometimes neurobiological factors. With practice and support, emotional awareness can grow—our journaling starter is here.
The Psychological Impact of Alexithymia
When inner signals are faint, decisions, boundaries, and relationships become harder. People may feel detached, misunderstood, or “numb.” Over time, the gap between life’s demands and inner guidance fuels stress, which can contribute to anxiety or low mood. Because expressing needs is tougher, conflicts linger and intimacy suffers—leading to isolation, or a sense of performing rather than connecting. If this sounds familiar in your partnership, try these relationship tips for alexithymia.
Common Causes of Alexithymia
- Early environment: Families that minimize or punish feelings teach children to suppress or ignore internal cues.
- Stress & trauma: Overwhelm can narrow attention to survival signals; the body stays vigilant while feeling-words go quiet. Learn about trauma-focused options like EMDR here and a broader PTSD treatment overview.
- Neurobiological factors: Differences in interoception and networks linking body sensations to emotion-language can shape awareness.
- Co-occurring conditions: Alexithymia can appear across diagnoses (e.g., trauma-related disorders, neurodevelopmental differences). Treatment still focuses on skills and support.
Diagnosis: How Is Alexithymia Identified?
Clinicians combine conversation, behavioral observation, and questionnaires to understand a person’s experience. One commonly used measure is the Toronto Alexithymia Scale (TAS-20), which screens difficulties in identifying and describing feelings and externally oriented thinking. Results help guide treatment targets (e.g., emotion labeling, interoception, communication), but clinical context matters more than any single score. Curious about temperament (not a diagnosis)? Try our quick 5-minute neuroticism test.
Ready to explore a plan? Book a callback at TherapyDial to discuss a tailored evaluation and next steps.
Effective Therapeutic Approaches for Alexithymia
Psychoeducation & Emotion Literacy
Learning the language of feelings is foundational. Therapists often introduce curated emotion word lists, “feelings wheels,” and simple check-ins (What am I feeling? Where do I notice it? What does it urge me to do?). Visual aids and values exercises make abstract feelings concrete. For a gentle start, use this journaling routine for emotional numbness.
CBT (Cognitive Behavioral Therapy)
CBT maps links among thoughts, feelings, bodily sensations, and behaviors. For alexithymia, CBT targets “externally oriented” habits by training attention inward, expanding emotion labels, and testing new communication behaviors. Homework might include emotion journaling, graded sharing with trusted people, and values-based decision practice. See our CBT overview here and try three DIY exercises to challenge thinking traps here.
Emotion-Focused Work
Emotion-focused approaches help clients contact, tolerate, and transform feelings in session—moving from vague unease to specific, workable emotions (e.g., from “bad” to “sad and disappointed”). Therapists pace exposure to feelings and model compassionate curiosity. Relationship-specific tips are here.
Trauma-Informed Therapy
When trauma contributes, phased care emphasizes safety and skills before deeper processing. Some people benefit from treatments referenced in the NICE PTSD guideline or modalities like EMDR (NYC explainer). Broader local support options are summarized here.
Group & Family Therapy
Groups provide practice reading others’ cues and sharing feelings in a supportive setting. Family sessions strengthen shared language, reduce misinterpretations, and align on supportive responses (“When I seem flat, try asking for sensations first: ‘Where do you feel it?’”). If social fear is part of the picture, try these 5 home CBT techniques.
CBT for Emotional Awareness: What It Looks Like
- Cognitive restructuring: challenge all-or-nothing, hyper-practical thoughts that crowd out emotions; replace with flexible, descriptive language—practice with our DIY distortion drills.
- Behavioral activation: schedule meaningful, varied activities; track body signals and mood before/after to build interoception and preference clarity.
- Skills worksheets: ABC charts (Activating event, Beliefs, Consequences), feeling/sensation logs, and values mapping. If journaling feels hard, start here.
- Communication drills: brief scripts: “I feel emotion when situation. I need specific request.”
Tip: Start with a two-word check-in twice a day: one emotion word + one body sensation. Keep it simple and consistent.
The Role of Mindfulness and Interoception
Mindfulness builds the capacity to notice internal signals without judgment. Evidence summaries from NCCIH describe benefits for stress, sleep, and mood. For alexithymia, mindfulness is adapted to emphasize interoception—awareness of body sensations that precede emotion words. If sleep is a blocker, consider a structured reset with CBT-I, and if anxiety spikes at home, these at-home CBT techniques can help.
- Body scan (3 minutes): slowly move attention from feet to face; name one sensation per region.
- Breath ratio 4-6: inhale 4 counts, exhale 6 for 2 minutes to downshift arousal.
- Noting practice: label “warm,” “tight,” “buzzing,” then pair a feeling word when ready.
- Self-compassion breaks: place a hand on chest; say, “This is hard. I’m not alone. May I be kind to myself.” (See the Center for MSC.)
Support Groups: Connecting with Others Facing Similar Challenges
Groups reduce isolation and offer live practice reading cues and sharing feelings in low-stakes settings. Members swap techniques (e.g., “sensation lists,” “color-coded emotion wheels”) and accountability for daily check-ins. Online formats can help those who prefer gradual exposure to sharing.
Lifestyle Changes that Reinforce Treatment
- Movement: brisk walks or yoga 3–5×/week; note “before/after” sensations to link body states to feelings.
- Sleep: regular bed/wake times; dim lights early; keep a 2-line sleep/mood note each morning—use this 14-day CBT-I reset if needed.
- Stress: combine short breathing breaks with longer strategies in our science-backed stress guide.
- Joy blocks: short, predictable activities that reliably evoke positive emotion (music, nature, creative play). If overwhelm is part of the mix, case studies on how ASMR helps are here.
A Gentle 8-Week Roadmap to Unlock Emotions
Week 1: Orientation
Learn emotion words & start 2×/day two-word check-ins (feeling + sensation). Set therapy goals at TherapyDial.
Week 2: Body Awareness
Daily 3-minute body scans; build a personal “sensation dictionary.”
Week 3: Language & Values
Expand emotion vocabulary; map top 5 values; try a small values-aligned action. If motivation is low, try a brief journaling prompt like this.
Week 4: Communication
Practice “I feel… when… I need…” with one trusted person. If social anxiety shows up, try these five CBT tools at home.
Week 5: Behavior Experiments
Test new ways of responding to triggers; journal the effect on sensations and mood (see thinking traps to watch).
Week 6: Meaning-Making
Connect patterns (“When I skip sleep, I feel blank.”) and adjust routines with CBT-I if needed.
Week 7: Deepening
Introduce compassion practices or begin trauma-informed work if appropriate (overview of EMDR here).
Week 8: Maintenance
Lock in 10-minute daily ritual: body scan → label → share or journal → one kind action.
Real-Life Mini-Examples (Names Changed)
“Numbers, Not Feelings”
Jordan, a finance lead, described problems in data terms but couldn’t voice emotions. With a daily two-word check-in and a 10-minute values exercise, they identified “anxious + tight jaw” before tough meetings and practiced a script to request clarity. Within a month, their partner reported more transparency and fewer conflicts.
“The Flat Line”
Maya felt “nothing” most days. In therapy, she started with sensation logs, then added a “three good things” gratitude practice and brief social exposures (two texts per day). After four weeks, she could label “content” and “relieved,” and began asking for support during deadlines.
“The Body Keeps the Scoreboard”
Sam had GI flares with no medical cause identified. Logging food, sleep, stressors, and sensations revealed spikes after criticism. CBT reframing plus self-compassion breaks and post-meeting walks reduced flares and improved sleep.
FAQs
Is alexithymia a diagnosis or a trait?
It’s best understood as a trait-like dimension—a tendency toward lower emotion awareness and expression—that can occur across diagnoses. Treatment targets skills, habits, and relational support rather than a single label. For a plain-English primer, see The Emotion Blindspot.
How do professionals assess alexithymia?
Through conversation, observation, and questionnaires such as the TAS-20. Scores inform goals (e.g., emotion labeling, interoception) but are interpreted within your life context. If you’re curious about temperament (not diagnosis), try our 5-minute neuroticism test.
Which therapies help the most?
CBT and emotion-focused approaches are common. If trauma is relevant, trauma-informed modalities may be integrated by a trained clinician (overview of EMDR here).
Are mindfulness and meditation actually helpful?
Mindfulness builds attention to internal signals and can reduce stress. See the NCCIH overview. Practices should be gentle, brief, and paired with self-compassion. If anxiety rises at home, try these CBT tools.
Where can I learn emotion words?
Therapists often use feelings wheels and graded lists. You can start by noting one emotion and one body sensation twice a day and bring those notes to therapy. If you feel “numb,” this journaling guide can help.
When to Seek Support Immediately
If you’re thinking about harming yourself or feel unable to stay safe, seek help now. Call your local emergency number or visit the nearest ER/ED. In the U.S., call or text 988 for the Suicide & Crisis Lifeline.